What Recent (but Enduring) Changes in the Healthcare Industry Mean for You
How many times have you heard the phrase “new normal” recently? Have you wondered what, exactly, that may look like for operators in the Healthcare space?
It’s too early to call every 2020 trend a winner or loser, but there are some sure-fire early takeaways for Healthcare industry players.
All business leaders in our industry – from independent labs to imaging centers, pharmacies, medical device developers, specialist practitioners, rehab facilities, CCRCs, dentists, and everything in between – are looking for the ratified lessons we’ve learned so far.
To get a handle on the takeaways, we caught up with Old National's top Healthcare Commercial Banking expert Don Woods, who shared five seismic (and lasting) shifts he’s seen within the senior care industry specifically.
He also explained why these changes are permanent, how they apply to other Healthcare sectors, and exactly what each one means to you and your niche. Let's listen in.
#1. Senior housing providers have redefined “quality”
No global event – not even a pandemic – can change the fact that Baby Boomers are still aging in unquestionably massive numbers. For the last ten years, over 10,000 people have been turning 65 years old each day. And the trend isn’t slowing. According to the most recent census, we can expect another ten years of that dramatic pattern.
While the pandemic can’t change that, it has forever transformed how consumers of Healthcare define excellence. “While the pandemic is, of course, tragic, it has also sped up a lot of innovative thinking in our industry,” says Woods. “There are some exciting developments on the horizon despite – partly because of – the pandemic.”
To answer these new developments, leading proprietors are no longer waiting for government aid to pivot and source PPE, testing, and logistics help and instead, investing in themselves.
For example, the operators who provide the best care have noticed the need for a counterbalance to the social impact 2020 has had on the senior population, and they’ve taken action. To restore some pre-pandemic social connections, senior housing operators have adopted new mobile devices, tablets, and apps. Previously, a lack of confidence and feelings of inadequacy contributed to the belief that seniors are less technologically savvy and can’t benefit from devices and software programs as much. But these tools are now mitigating the distance and obstacles between patients and the world.
- They allow residents and patients to experience video calls with loved ones.
- They enable people to communicate internally without having to be face-to-face (for example, caregiver collaboration and suitemate interactions)
- They let people order food and make appointments.
- They empower patients to competitively challenge one another in mentally stimulating digital games.
- They provide a creative outlet to people who want to produce and publish their own content.
- They give folks the medium to consume that content, whether it’s self-help encouragement, inspiring stories, how-to crafting tutorials, or lighthearted entertainment.
- They facilitate medical checkups with offsite practitioners.
Technology is only one way the best operators stand out today. Solving the social conundrums of the pandemic (in this case, with tablets and apps) is just one indication of overall innovative thinking. But it’s that mindset that now separates those providers who will thrive from those who will struggle or even fade away.
Consider this: occupancy across all senior communities is still dropping as areas deal with the Covid-19 disruption. However, investor behavior and analysis indicates the dip is a temporary change. And when the dust begins to settle, we’ll see some consolidation and even merger-and-acquisition activity that exposes which entities invested while others hunkered down, resisting the capital investments it takes to provide true quality care.
#2. Telehealth is yesterday’s luxury, today’s necessity, and tomorrow’s utility
Not long ago, only the most extreme circumstances warranted and permitted remote care. Today, it’s a lifesaver. Soon, it will simply be the accepted way of doing things.
Regulation, implementation, and administration previously hindered telemedicine. A global health event changed all of that overnight.
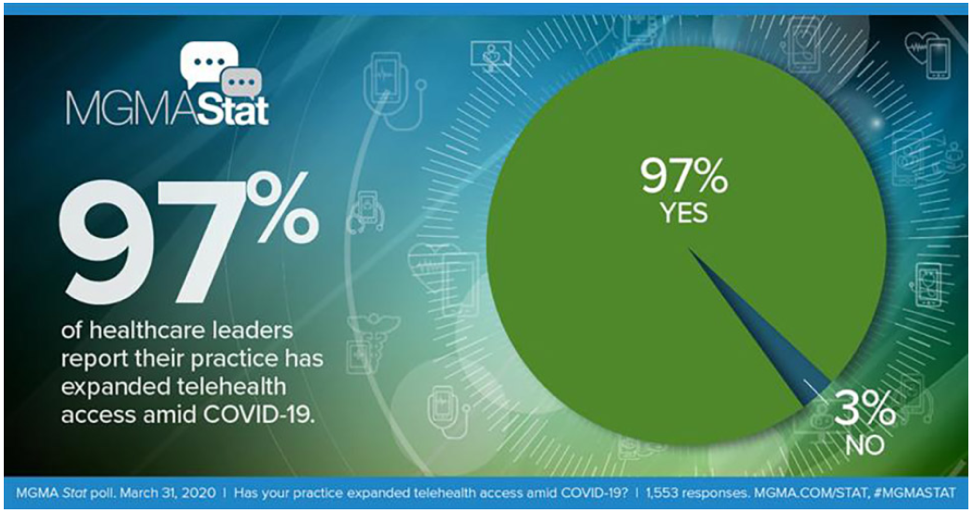
From February to June of 2020, physician usage of telehealth surged from 10% to 64%. A survey conducted by the Medical Group Management Association found that only 3% of Healthcare leaders report not expanding telehealth access amid the global health event.
Source: Medical Group Management Association
“Telehealth will never replace an actual physical visit from a doctor or nurse practitioner,” explains Woods. “But telehealth enhances the relationship by providing a real-time visual where doctors and nurses can actually speak with the person.”
From there, Woods goes on; the experts can listen to people discuss their symptoms, observations, and questions. Throughout the meeting, practitioners can observe the individuals’ body language and speech, applying their experience to catch things that may change from one visit to the next. “There's software now that enables people to use an iPad to take their temperature,” says Woods with a smile. “It's unbelievable.”
The change allows for a few accompanying benefits. First, it allows practitioners and care providers to scale operations, rerouting many resources previously allocated to in-person routine visits. It also improves the customer experience, generating a positive feedback loop that synergistically benefits everyone involved. And finally, it’ll serve to catch and address problems earlier for advance intervention, an elusive goal that has historically perplexed the medical community.
How do we know the change is an enduring one? The CDC reports that 93% of recent telehealth visits were not Covid-related. This speaks to the lasting nature of telehealth’s adoption and the tactic’s scope of usefulness across sectors in the medical industry.
#3. Elective procedures and screenings are back – and will soon outperform previous totals
With one eye ever on Covid surge capacity and local case counts, facilities can now address what the University of Michigan Health Lab calls the “Surgery Backlog.” Priority will, of course, go to category one and two non-urgent but necessary procedures like cancer operations and organ donations. Surgeons will also strategically rank their backlog in order of how resource-intensive each treatment type is.
But soon, procedures like hip and knee replacements will re-enter the conversation – and eventually, they’ll surpass their pre-pandemic numbers. Experts at the World Health Organization explain why:
“A longer life brings with it opportunities, not only for older people and their families but also for societies as a whole. Additional years provide the chance to pursue new activities such as further education, a new career, or pursuing a long-neglected passion. Older people also contribute in many ways to their families and communities. Yet the extent of these opportunities and contributions depends heavily on one factor: health.”
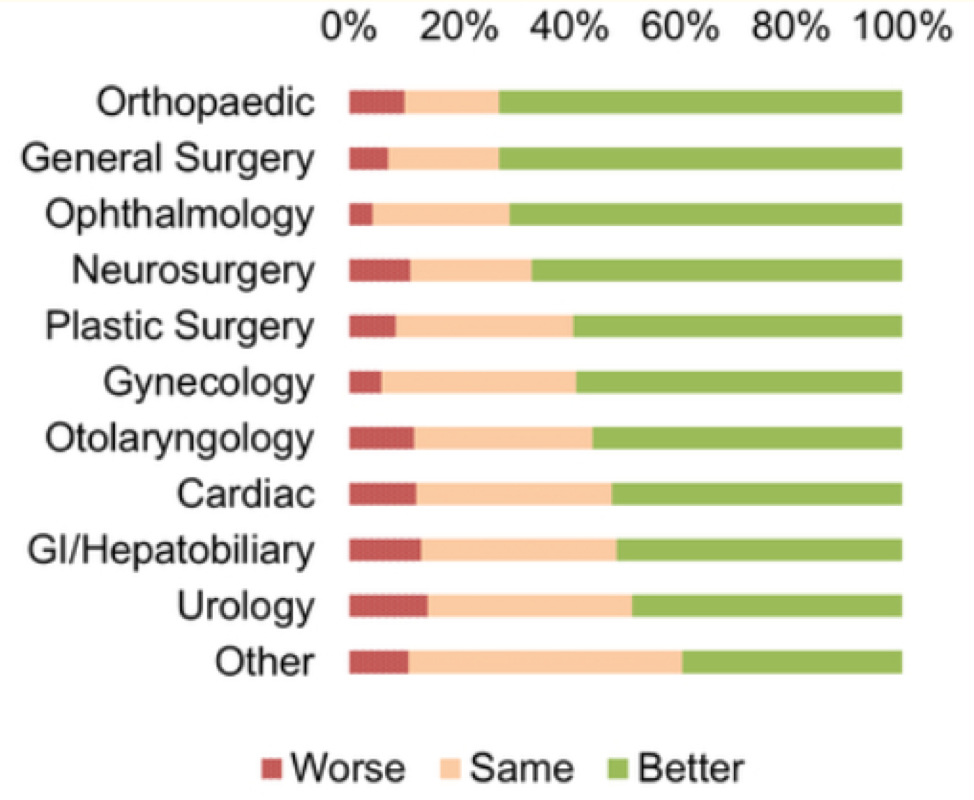
A recent study published by the National Institutes of Health reveals that an average of 61% of people who underwent an elective procedure reported a higher quality of life across surgery types.
Source: US National Institutes of Health
In a way, the first two trends we discussed – operator innovation and telehealth adoption – are enabling the upcoming wave of elective procedures. Without the increase in quality care of older adults and the more frequent virtual communication and collaboration among all individuals and providers, elective procedures wouldn’t be in such a position to flourish.
#4. Newly designed experiences start with the physical
As Woods mentioned, virtual care is on the rise, but it’ll never replace in-person services. In fact, those in-person experiences are undergoing a transformation of their own.
“Here’s another trend that started well before Covid-19, but was greatly accelerated by the pandemic,” says Woods. “You used to see these big dining rooms and large congregate areas, but meanwhile, living spaces were relatively small. Soon, you're going to see beefier living spaces in the future.”
Woods says the larger style private rooms and suites are leading the way in skilled care facilities, but the shift will now extend to the independent living, assisted living, and memory care segments.
We’ll also see the short-term pandemic policies and fixes inspire larger, more permanent design changes like…
- Hand-delivered meals replacing buffet-style service.
- Permanent — not temporary plexiglass — dividers in reception and visitation areas.
- Drive-up porticos specifically for safely distanced in-person visits.
- Replaced, upgraded heating, ventilation, and air conditioning systems for better airflow and less — even eliminated — recirculation.
- Intelligent, data-enabled isolation wings.
- A resurgence of green spaces and open-air functional areas for more time outdoor.
- Accessible, transparent tier-one, -two, and -three structural surge plans on hand for individuals, visitors, caregivers, and inspectors to view.
- New doctor and specialist office visit procedures like online form completion, in-vehicle check-ins, and pre-visit phone screenings to assess symptoms.
- One-way foot traffic and separate entrances/exits for incoming and outgoing navigation.
Woods says that as families start navigating their future plans, they need to consider these new developments — architectural safety measures that most alternative arrangements won’t provide. “When that consideration comes around that mom or dad needs assistance, it’s often going to be better for your senior loved one at a facility that's addressing these items,” he says. “Consider all these new measures and protocols as opposed to, for example, moving in with another loved one. The typical household still has people coming in and out of the home, kids that are still going to school, and other factors outside of your control.”
#5. The government relaxes some regulations while imposing new ones
One final enduring change to note is the government’s role in helping businesses navigate the ever-evolving developments from this pandemic, as well as public sentiment and behavior. As new information becomes available, recommendations and regulations will continue guiding operators.
The Centers for Medicare and Medicaid Services provides a full list of waivers issued to Healthcare providers since the federal government issued an emergency declaration in early 2020. Many restrictions are temporarily (or even permanently) nullified, including video requirements on many telemedicine appointments and the requirement for Medicaid patients to be under the care of a primary physician.
Thankfully, experts at the American Medical Association have broken down the CDC’s new non-Covid-Care framework into an actionable, 14-step guide that ensures a successful (and compliant) recommencement of routine care.
Source: American Medical Association’s “COVID-19: A physician guide to keeping your practice open.”
Woods says that the tactical takeaway for practitioners is to revisit your operations’ business model, costs, and cash flow. “There are going to be added expenses,” he says. And while PPE compliance and infection control measures will play a role, the talent required to administer the new normal will impact your bottom line the most. “The biggest expense we're going to see is on the human resource side. Skilled talent will require higher wages across the industry because there are legitimate risks and safety concerns involved.”
As a byproduct of that initial compensation increase, says Woods, the supportive, non-medical roles will earn higher wages as well. “When primary wages do increase in the industry, you're going to see other people coming into your sector that have other creative talents,” he says. “For example, your marketing people – you’ll now have a role for somebody that knows how to do social and digital advertising, and they’ll be worth more, too. It's going to change the paradigm of a lot of facilities.”
The more things change, the more they stay the same
Woods says that many operators in the Healthcare industry are entrepreneurs at heart – they’ll always see challenges as opportunities. “This global health event has accelerated a lot of things. It's brought a lot of things to light,” he says. “There will be many changes that will come as a result of this. So now that we're getting past the initial storm, we should be looking at the silver linings and capitalize on the positive opportunities that are coming out of this.”
To learn exactly how you can capitalize on emerging developments, contact the Healthcare team of commercial experts at Old National Bank today.